If you’ve ever dealt with deep, painful breakouts along your jawline that seem to appear like clockwork before your period, you know how frustrating hormonal acne can be. Unlike the T-zone breakouts of your teenage years, this type of acne often doesn’t respond to basic skincare alone.
The good news? Research from the past decade suggests that certain vitamins and minerals can meaningfully support your skin when used strategically. The key word here is “support”not cure, not replace proper treatment, but genuinely help reduce inflammation, balance hormone metabolism, and accelerate healing.
In this guide, you’ll learn which nutrients have the strongest evidence behind them, how to use them safely, and how to combine them with diet, lifestyle, and skincare for the best possible results. Whether you’re dealing with mild cyclical breakouts or more stubborn cystic acne, understanding the role of vitamins for hormonal acne can be a game-changer for your skin health.
Key Takeaways on Vitamins for Hormonal Acne
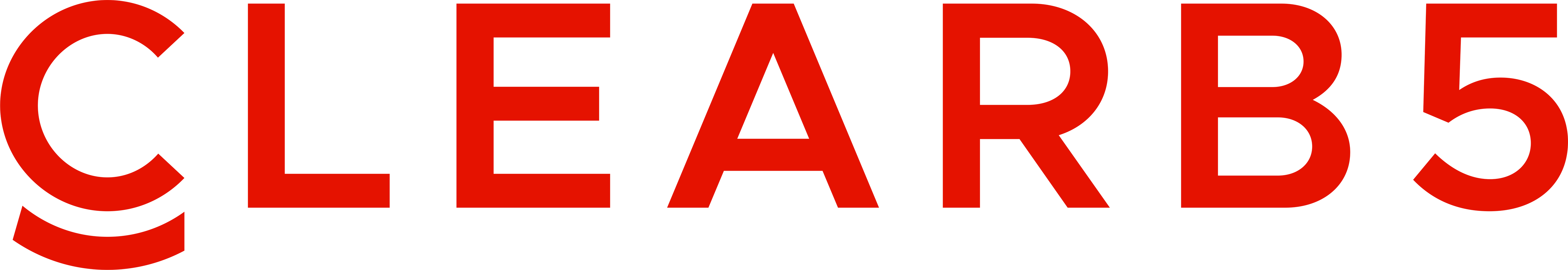
- Hormonal acne is driven by complex hormonal and inflammatory pathways. Correcting vitamin D, zinc, omega-3, and antioxidant status can meaningfully support skin clarity and reduce acne breakouts.
- Vitamins and supplements are tools, not magic bullets. Best results come from combining them with balanced nutrition, stress management, solid skincare, and dermatologist-prescribed therapies when needed.
- Safety first. Avoid megadoses, be cautious with pregnancy and chronic illness, and always disclose your supplements to your healthcare provider.
- Start simple and be consistent. Choose one or two evidence-backed changes (e.g., vitamin D + zinc, or omega-3s + probiotics) and stick with them for at least 2–3 months before assessing results.
- Improvement is possible. Many adults see significant clearing of hormonal acne over time with a personalized, science-informed plan that includes smart vitamin use alongside proper skincare and lifestyle support.

Quick Answer: Can Vitamins Really Help Hormonal Acne?
Let’s cut to the chase: vitamins and minerals cannot “cure” hormonal acne on their own. However, when used alongside proper skincare and medical treatment (if needed), they can reduce skin inflammation, support hormone metabolism, and improve how quickly your skin heals from breakouts. Think of them as powerful supporting players rather than the entire team.
The evidence is strongest for correcting actual deficiencies. If you’re low in vitamin D, zinc, or omega-3 fatty acids, which many adults are, bringing those levels up can make a noticeable difference in acne severity.
Here’s what the research supports:
- Best-studied nutrients for hormonal acne: Vitamin D, vitamin A (and prescription retinoids), zinc, vitamin C, vitamin E, B-complex vitamins (especially B6), omega-3 fatty acids, myo-inositol, and probiotics
- Who may benefit most: People with PCOS, irregular menstrual cycles, or adult-onset jawline acne, particularly those with documented low vitamin D, zinc, or omega-3 intake
- Timeline for results: Most studies evaluate outcomes at 8–12 weeks, so patience is essential
- Critical safety note: Avoid megadoses of vitamin A or B12 without medical supervision, as these can cause serious side effects or even worsen breakouts
What Is Hormonal Acne?
Hormonal acne is a form of acne vulgaris driven primarily by fluctuations in hormones, specifically androgens like testosterone and DHEA-S, as well as the hormones estrogen and progesterone. Unlike typical teenage acne that clusters in the T-zone, hormonal breakouts tend to appear on the jawline, chin, lower cheeks, and sometimes the neck.
This type of inflammatory acne commonly affects women in their 20s through 40s and tends to follow predictable patterns:
- Flaring 5–10 days before menstruation
- Worsening during high-stress periods
- Appearing after stopping birth control
- Persisting in women with polycystic ovary syndrome (PCOS)
- Emerging during perimenopause (late 30s–50s)
How Hormonal Acne Develops
The mechanism behind hormonal breakouts follows a chain reaction:
- Androgens increase sebum production in your sebaceous glands
- Excess sebum mixes with dead skin cells, creating clogged pores
- C. acnes bacteria proliferate in this oxygen-poor environment
- Your immune system responds with inflammation, producing papules, pustules, and cystic acne lesions
Here’s an important connection: insulin resistance and elevated insulin levels (common in PCOS or high-sugar diets) can increase androgen production indirectly. This is why blood sugar balance matters so much for hormonal breakouts.
Vitamins for hormonal acne work by supporting hormone metabolism, improving immune balance, and strengthening your body’s antioxidant defenses, not by directly “killing” acne bacteria. They address the upstream factors that make your skin more vulnerable to breakouts in the first place.
Key Vitamins and Minerals That May Help Hormonal Acne
This section covers the nutrients with the most research behind them for acne and hormone-related skin issues. Most evidence comes from small clinical trials and observational studies conducted between 2000 and 2023, so results vary from person to person.
What you’ll find below:
- Specific mechanisms of action for each nutrient
- Practical food sources you can incorporate today
- Typical supplemental dose ranges based on published research
- Key safety cautions to keep you protected
Let’s dive into each one.
Vitamin D
Vitamin D deficiency is remarkably common in acne patients. Multiple studies between 2014 and 2021 have found that people with moderate to severe acne tend to have significantly lower 25(OH)D levels compared to those with clear skin.
Small clinical trials from 2016–2017 showed promising results: supplementing with 1,000–2,000 IU of vitamin D3 daily for 8–12 weeks reduced inflammatory acne lesions and improved insulin sensitivity in participants with both acne and PCOS.
How vitamin D helps:
- Modulates immune response in the skin
- Reduces production of pro-inflammatory cytokines
- May help normalize oil production in sebaceous glands
- Supports overall skin barrier function
Food sources:
- Midday sun exposure (10–30 minutes depending on skin tone)
- Fortified dairy or plant milks
- Fatty fish (salmon, mackerel, sardines)
- Egg yolks
- OTC vitamin D3 supplements
Dosing guidance: For most adults, 1,000–2,000 IU daily is a reasonable range. Ideally, get your blood levels tested first, optimal 25(OH)D is typically 40–60 ng/mL. Long-term doses above 4,000 IU daily should only be used with medical supervision to avoid hypercalcemia.
Who’s at higher risk for deficiency: People with darker skin tones, those living at high latitudes (UK, Canada, Northern US in winter), and anyone who spends limited time outdoors.

Vitamin A (and Retinoids)
Vitamin A is the parent vitamin of prescription retinoids like tretinoin and isotretinoin—which are gold-standard treatments for severe acne and cystic acne. This nutrient plays a central role in skin cell turnover and sebum regulation.
Older studies from the 1970s–1990s tested oral vitamin A at doses of 25,000–50,000 IU daily and found reductions in acne lesions. However, these high doses also caused significant side effects, which is why prescription isotretinoin (a controlled retinoid) became the preferred medical option.
How vitamin A works:
- Reduces sebum output from sebaceous glands
- Normalizes keratinization (skin cell turnover) to prevent clogged pores
- Has direct anti-inflammatory effects within hair follicles
Food sources:
- Liver (extremely high in vitamin A—one serving exceeds daily needs)
- Eggs and butter
- Provitamin A carotenoids: carrots, sweet potatoes, kale, spinach
Critical safety warning: High-dose vitamin A supplements can cause liver toxicity, severe headaches, and birth defects. Never use high-dose oral vitamin A during pregnancy or when trying to conceive.
Practical recommendation: For most people concerned with hormonal acne, focusing on a carotenoid-rich diet and discussing prescription topical retinoids with a dermatologist is far safer than taking high-dose oral vitamin A supplements. Topical vitamin A derivatives (like adapalene, available over-the-counter) offer acne treatment benefits without systemic toxicity risks.
Zinc
Zinc is one of the best-studied minerals for acne, with research dating back to the 1970s. Studies have consistently shown that oral zinc supplementation can modestly reduce inflammatory acne lesions, sometimes with effects comparable to low-dose antibiotics.
How zinc helps:
- Powerful anti-inflammatory properties
- Antioxidant effects that protect skin cells
- Reduces C. acnes bacterial growth
- Helps regulate sebum production and keratinization
Research dosing: Clinical studies have used anywhere from 30 mg to 90 mg of elemental zinc daily. Common forms include zinc gluconate, zinc sulfate, and zinc picolinate. It’s important to understand the difference between salt weight and elemental zinc, for example, 220 mg of zinc sulfate contains about 50 mg of elemental zinc.
Safe self-supplementation range: 15–30 mg elemental zinc daily for adults, taken with food to reduce nausea. Chronic intake above 40 mg elemental zinc daily can lead to copper deficiency and anemia over time.
Food sources:
- Oysters (the richest source by far)
- Red meat and poultry
- Pumpkin seeds
- Chickpeas and other legumes
- Fortified cereals
Important tip: If taking zinc supplements for longer than 2–3 months, consider pairing with a small amount of copper (1–2 mg daily) under healthcare guidance to prevent imbalance.
Vitamin C
Vitamin C doesn’t directly “fix” hormones, but it plays crucial supporting roles in skin healing that are especially relevant for hormonal breakouts. This water-soluble antioxidant is essential for collagen production, wound healing, and protecting skin from free radical damage.
How vitamin C supports hormonal acne recovery:
- Accelerates healing of acne lesions
- Reduces post-inflammatory hyperpigmentation (those dark marks left behind)
- Provides antioxidant protection to stressed skin
- Supports collagen synthesis for skin repair
Topical vs. oral: Most acne-specific research focuses on topical vitamin C (10–20% L-ascorbic acid serums), which has strong evidence for brightening and reducing pigmentation from acne scars. Oral vitamin C supports systemic antioxidant defenses but isn’t a direct acne treatment.
Food sources:
- Citrus fruits (oranges, grapefruit, lemons)
- Berries (strawberries, blueberries)
- Kiwi
- Bell peppers
- Broccoli and Brussels sprouts
- Tomatoes
Dosing guidance: A typical oral intake of 200–1,000 mg daily from food plus supplements is generally safe. Amounts above 2,000 mg daily can cause digestive upset in some people.
Best approach: Combine adequate oral vitamin C intake with daily sunscreen and a gentle topical vitamin C serum to maximize benefits for hormonal acne marks and support overall skin health.
Vitamin E
Vitamin E is a fat-soluble antioxidant that protects skin lipids from oxidative stress and supports skin barrier function. Small studies from the 1990s through 2010s have found lower blood levels of vitamin E in acne patients compared to those with clear skin, suggesting that chronic skin inflammation depletes antioxidant reserves.
How vitamin E helps:
- Protects cell membranes from oxidative damage
- Supports healthy skin barrier function
- Works synergistically with vitamin C for enhanced antioxidant protection
- May help reduce inflammation in existing acne
Food sources:
- Sunflower seeds
- Almonds and hazelnuts
- Avocado
- Olive oil
- Wheat germ oil
Dosing guidance: For most people, 15 mg (22.4 IU) of vitamin E daily from diet and a multivitamin is sufficient. Avoid taking high-dose vitamin E supplements (above 400 IU daily) without medical advice, as there’s potential bleeding risk in certain populations.
Pro tip: Combining vitamins C and E, whether through diet or supplementation, may offer synergistic antioxidant support for skin stressed by chronic hormonal breakouts.
B-Complex Vitamins (Especially B6)
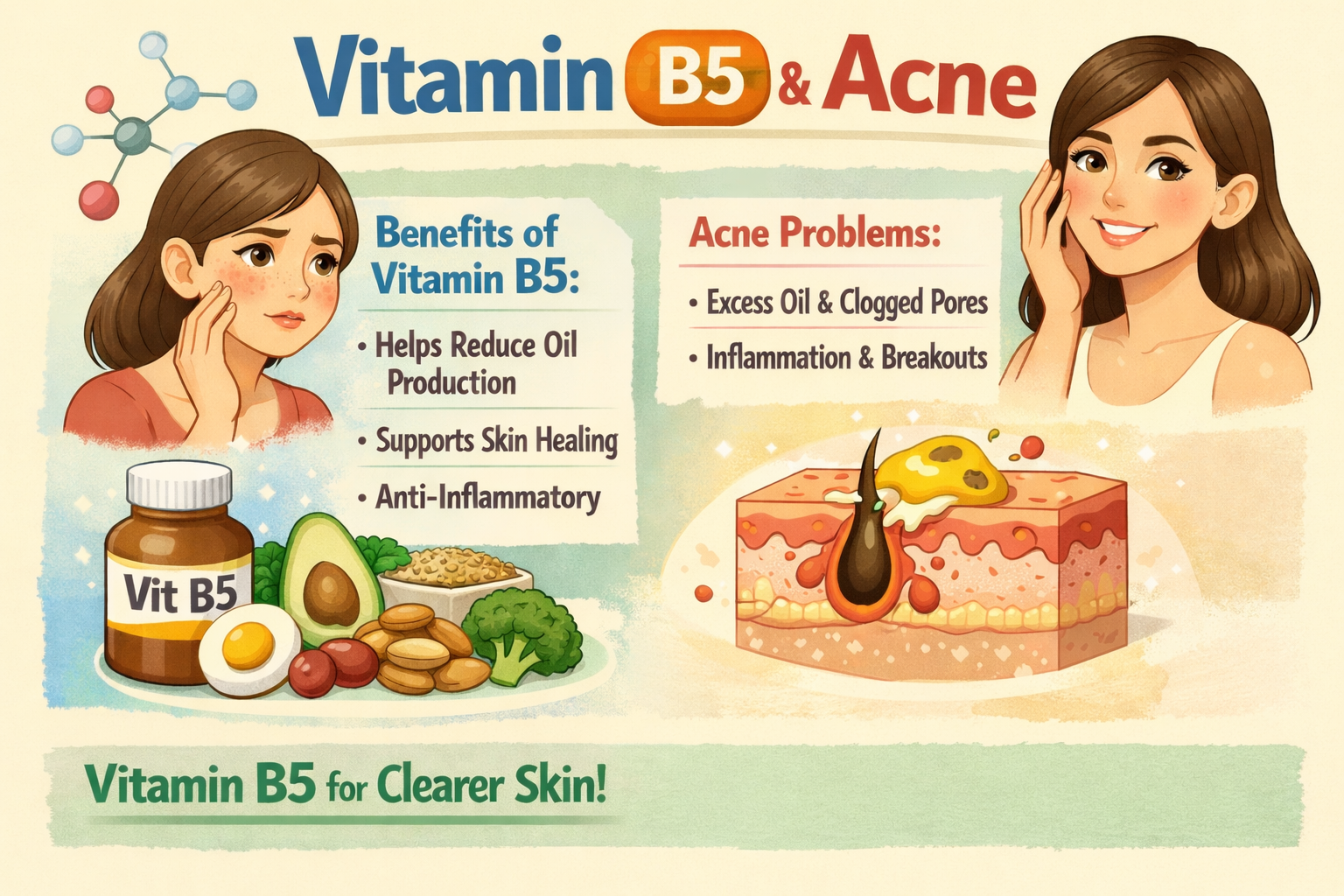
The B vitamins are involved in energy production, methylation, and liver detoxification pathways that metabolize hormones, including estrogen metabolism and androgen processing. However, the relationship between B vitamins and acne is nuanced, some help, while others can actually trigger breakouts.
Vitamin B6 (pyridoxine) deserves special attention for hormonal acne. It supports progesterone synthesis and may help balance estrogen dominance, which is sometimes associated with premenstrual acne flares.
Pantothenic acid (B5) has shown promise in one small trial where 4.4 g daily for 12 weeks reduced inflammation and improved quality of life in acne patients.
The B12 warning: Several case reports from 2015–2020 have linked high-dose B12 injections or supplements to new acne breakouts. Research suggests B12 may alter gene expression in C. acnes bacteria, increasing inflammatory porphyrin production. If you notice acne worsening after starting B vitamins, high-dose B12 may be the culprit.
Food sources for B vitamins:
- Whole grains
- Poultry and fish
- Eggs
- Leafy greens
- Legumes
- Nutritional yeast
Dosing guidance: Use moderate-dose B-complex supplements that stay near the RDA (e.g., B6 at 2–10 mg daily) rather than megadoses. Avoid additional high-dose B12 if you notice new breakouts appearing after starting supplementation.
Bottom line: B-complex vitamins are best used to correct suspected deficiency (fatigue, low appetite, mouth sores) rather than as a stand-alone acne vitamin solution.
Other Helpful Nutrients for Hormonal Acne
Beyond classic vitamins and minerals, certain nutrients have emerging evidence for supporting hormone balance, insulin sensitivity, and inflammation relevant to hormonal acne. These hormonal acne supplements should be used more cautiously, often with guidance from a healthcare provider, especially for those with PCOS, on medications, or planning pregnancy.
Omega-3 Fatty Acids (Fish Oil & Plant Sources)
Omega-3 fatty acids (EPA and DHA) reduce systemic inflammation throughout the body, including the skin. Small trials from 2008–2014 found that omega-3 supplementation, combined with standard topical care, reduced inflammatory acne lesion counts.
How omega-3s work:
- Modulate inflammatory eicosanoids (signaling molecules)
- Improve skin barrier function
- Make hormonal breakouts less red, swollen, and painful
- Support gut health, which indirectly influences skin
Food sources:
- Oily fish (salmon, sardines, mackerel)
- Flaxseed and chia seeds
- Walnuts
- Algae oil (vegan EPA/DHA option)
Dosing from research: 1,000–3,000 mg combined EPA+DHA daily. Consult a doctor if you’re on blood thinners or have bleeding disorders.
Timeline: Consistent intake over at least 8–12 weeks is needed before judging benefits for acne.
Myo-Inositol
Myo-inositol is a B-vitamin-like compound frequently used in PCOS management to improve insulin sensitivity, lower androgens, and promote regular ovulation. Clinical trials from 2007–2020 in women with PCOS showed that 2–4 g daily improved insulin markers, reduced free testosterone, and often improved acne and excess hair growth as secondary outcomes.
How myo-inositol works:
- Improves insulin signaling pathways
- Reduces ovarian androgen production
- Decreases the downstream sebum stimulation that drives hormonal acne
Food sources (smaller amounts):
- Citrus fruits
- Beans and legumes
- Whole grains
- Nuts
Therapeutic doses require supplementation, you can’t get enough from food alone.
Typical dosing: 2 g myo-inositol twice daily, often combined with 200 mcg folate, under medical supervision.
Cautions: Generally well-tolerated but can cause mild GI upset. Those with bipolar disorder should consult their psychiatrist, as inositol can interact with mood stability.
DIM (Diindolylmethane)
DIM is a compound formed when you digest cruciferous vegetables like broccoli, cabbage, and Brussels sprouts. It’s popular in supplements for hormonal balance and is sometimes used for acne related to estrogen dominance or post-pill breakouts.
Proposed mechanism: DIM may shift estrogen metabolism toward less inflammatory metabolites (2-hydroxyestrone) and away from potentially problematic 16-hydroxyestrone.
Evidence reality check: Human data specifically for acne is limited, mostly from small open-label or company-sponsored trials.
Common supplement doses: 100–200 mg DIM daily.
Strong recommendation: Consult a healthcare provider before using DIM, especially if you have a history of estrogen-sensitive cancers or are on hormonal medications.
Food-first approach: Aim for 1–2 cups of cruciferous vegetables most days. Consider supplements only as a second-line option.
Probiotics
The gut-skin axis is real: imbalanced gut flora (dysbiosis) and increased intestinal permeability can raise systemic inflammation and influence insulin and hormone signaling that affect acne pathogenesis.
Small human studies from 2010–2016 found that specific probiotic strains improved acne severity and/or insulin sensitivity:
- Lactobacillus rhamnosus GG
- Lactobacillus casei
- Bifidobacterium bifidum
How balancing gut health helps skin:
- Competitive inhibition of pathogenic bacteria
- Reduced endotoxin levels entering circulation
- Improved intestinal barrier function
- Modulation of systemic immune responses
What to look for: Multi-strain products with at least 5–10 billion CFU. Evidence is strain-specific, so label details matter.
Food sources for probiotics:
- Yogurt with live cultures
- Kefir
- Kimchi and sauerkraut
- Miso
- Other fermented foods
Combine these with a high-fiber diet (prebiotics) to support gut diversity and lower systemic inflammation.
Caution: Those with IBS, SIBO, or immune compromise should consult a clinician before starting probiotic dietary supplementation.
Spearmint (Optional Herbal Support)
Small studies from the early 2010s suggest that drinking spearmint tea twice daily for 30 days lowered free testosterone and subjectively improved hirsutism and acne in some women with androgen excess.
The anti-androgen effect is mild but may be helpful as a gentle, low-risk herbal remedy for women with oily skin, unwanted facial hair, and cyclical jawline acne.
Typical use: 1–2 cups of spearmint tea daily.
Caution: People with low blood pressure or on sedative medications should check with a provider before heavy spearmint use. Essential oils or high-dose extracts require extra caution.
Berberine (Advanced Option, Especially for PCOS)
Berberine is a plant alkaloid found in barberry, goldenseal, and Coptis with strong evidence for improving insulin resistance, similar to metformin in some studies.
Small trials around 2012–2015 found that 1.0–1.5 g daily berberine in women with PCOS reduced androgens, improved ovulation rates, and often improved acne as a secondary effect.
How berberine works:
- Improves insulin sensitivity
- Lowers blood glucose and insulin levels
- Modulates gut microbiome composition
- May reduce systemic inflammation
Critical warning: Berberine is an “advanced” herbal supplement that should only be used under professional supervision. It can interact with many medications including antibiotics, blood thinners, and blood pressure drugs. It is not suitable during pregnancy.
Research doses: 500 mg 2–3 times daily with meals for 8–12 weeks—but this is not a DIY supplement. Work with a qualified practitioner.
How to Use Vitamins for Hormonal Acne Safely
Smart supplementation means avoiding common mistakes like megadoses, unsafe combinations, or guessing at what you need. Lab testing (vitamin D, B12, ferritin, fasting insulin) can personalize your approach rather than leaving you shooting in the dark.
If you have moderate to severe acne, PCOS, irregular cycles, or are on prescription medications, working with a dermatologist, endocrinologist, or integrative physician is essential before starting supplements for hormonal acne.
Smart Dosing and Timing Tips
Start one supplement at a time. Add a new one (e.g., zinc), wait 2–4 weeks, then consider adding another (e.g., omega-3s). This approach makes it clear what’s helping—or what’s causing side effects.
Timing matters:
|
Nutrient Type |
Best Timing |
|---|---|
|
Fat-soluble (vitamin D, E, fish oil) |
With meals containing healthy fats |
|
Zinc |
With food, but away from high-calcium meals |
|
Probiotics |
Empty stomach or as directed by manufacturer |
|
Water-soluble (vitamin C, B vitamins) |
Any time, with or without food |
Stay within safe ranges unless supervised:
- Vitamin D: up to 2,000 IU daily
- Zinc: up to 30 mg elemental daily
- Vitamin A: within multivitamin amounts unless prescribed by a doctor
Track your progress. Keep a skin diary noting cycle days, stress levels, supplements, and acne severity. Aim to identify patterns over at least 3 menstrual cycles (roughly 3 months) before drawing conclusions.
Recognizing Possible Deficiencies and Imbalances
These signs might hint at nutrient gaps relevant to hormonal acne:
- Frequent infections, fatigue: May suggest low vitamin D or zinc
- Dry or rough skin: Could indicate insufficient vitamin A or essential fatty acids
- Easy bruising, slow wound healing: Possible vitamin C insufficiency
- Heavy PMS and mood swings: Sometimes linked to B6 or magnesium gaps
These signs are non-specific and don’t replace blood tests. Before high-dose dietary supplements, ask your doctor for relevant labs.
Lab markers to consider requesting:
- 25-OH vitamin D
- Serum zinc
- B12 and folate
- Fasting insulin
- Lipid panel
- Sex hormones (free testosterone, DHEA-S) if PCOS is suspected
Re-test vitamin D and other relevant nutrients after 3–6 months of supplementation to avoid overshooting into toxicity.
Side Effects, Interactions, and Who Should Avoid Certain Vitamins
Main concerns:
- High-dose vitamin A: Risk of liver toxicity and birth defects
- High-dose vitamin E: Potential bleeding risk
- High-dose zinc: Nausea, copper deficiency with chronic use
- High-dose B12 or B6: Can trigger or worsen acne flare ups in susceptible individuals
Hormone-active supplements (DIM, berberine, vitex, spearmint) can interact with prescription hormones, blood sugar medications, blood thinners, and some antidepressants.
Groups requiring extra caution:
- Pregnant or breastfeeding women (no high-dose vitamin A, DIM, berberine, or vitex)
- People with liver or kidney disease
- Those on isotretinoin (already receiving high-dose vitamin A derivative)
- Anyone on multiple prescriptions
Best practice: Bring a complete list of all acne supplements (with doses and brands) to your dermatologist or GP before starting a new regimen.
Combining Vitamins with a Holistic Hormonal Acne Plan
Vitamins and supplements work best when paired with diet, lifestyle changes, and appropriate topical medications or prescription treatments. They are not stand-alone fixes for hormonal imbalances.
Realistic expectations:
- Mild to moderate hormonal acne may improve noticeably with a combined approach over 3–6 months
- Severe cystic acne usually needs prescription help—don’t delay seeking professional care
- Even “natural remedies” require consistency and patience
Diet and Blood Sugar Balance
What you eat directly impacts insulin, androgens, and inflammation—all key players in hormone balance and skin clarity.
Foods to emphasize:
- High-fiber vegetables (broccoli, leafy greens, cauliflower)
- Low-glycemic fruits (berries, apples, citrus)
- Whole grains and legumes
- Lean proteins (fish, poultry, tofu)
- Healthy fats (olive oil, avocado, nuts, seeds, oily fish)
Foods to minimize:
- Ultra-processed snacks and fast food
- Sugary drinks and desserts
- Frequent refined-carb snacks (white bread, pastries)
The dairy question: Some observational studies link cow’s milk (especially skim milk with high whey content) to acne. Evidence is mixed, but personal experimentation guided by a clinician or dietitian may be worthwhile if you suspect a connection.
Build nutrient-rich meals:
- Fatty fish twice weekly for omega-3s and vitamin D
- Pumpkin seeds for zinc
- Citrus and berries for vitamin C
- Colorful vegetables for carotenoids and antioxidants

Stress, Sleep, and Exercise
Chronic stress elevates cortisol, which can increase adrenal androgens and worsen hormonal acne. This explains why many people experience stress acne flares during exams, work deadlines, or emotional upheaval.
Sleep matters: Aim for 7–9 hours of consistent sleep nightly. Sleep deprivation disrupts insulin, cortisol, and appetite hormones that all influence healthy skin.
Stress management tools:
- Brisk walks or light cardio
- Yoga and stretching
- Breathwork exercises
- Journaling
- Mindfulness apps (10–15 minutes daily)
Exercise benefits: Regular moderate exercise (around 150 minutes weekly) improves insulin sensitivity and circulation, indirectly supporting hormone regulation and overall skin health.
Skincare and Medical Treatments
Even with optimal vitamin status, clogged pores and existing acne lesions still need topical treatments to clear.
Basic hormonal-acne-friendly routine:
- Cleanser: Gentle, non-comedogenic, twice daily
- Treatment: Salicylic acid or benzoyl peroxide for pore clearing and bacteria control
- Moisturizer: Non-comedogenic, supports skin barrier
- Sunscreen: Broad-spectrum SPF 30+ daily
Topical retinoids (adapalene, tretinoin) are especially effective for preventing clogged pores and comedones. They complement an internal vitamin A-rich diet but require guidance to minimize irritation and dry skin.
Prescription options for severe breakouts:
|
Treatment |
How It Works |
|---|---|
|
Combined oral contraceptives |
Suppress ovarian androgen production |
|
Spironolactone |
Blocks androgen receptors |
|
Metformin |
Improves insulin sensitivity (for PCOS) |
|
Isotretinoin |
Dramatically reduces sebum and treats severe acne |
These decisions should be made with a dermatologist or gynecologist based on your individual situation.
Don’t delay professional help if you have painful nodules, scarring, or acne that hasn’t improved after 3–6 months of lifestyle changes plus supplements.
Frequently Asked Questions About Vitamins for Hormonal Acne
Which vitamins are best for hormonal acne? The most evidence-backed options are vitamin D, zinc, and omega-3 fatty acids for inflammation and hormone support, with myo-inositol being particularly helpful for those with PCOS.
Can vitamins alone clear my hormonal acne? They may significantly improve acne in mild cases and support clear skin overall, but moderate to severe or scarring acne almost always requires prescription topical medications or systemic treatments.
How long do vitamins take to work for hormonal acne? Most studies evaluate results at 8–12 weeks. Track changes over at least three menstrual cycles before deciding whether a supplement is working for you.
Are there vitamins that can make acne worse? Yes, high-dose B12 and B6 have been linked to acne flares in some individuals. Excessive iodine (from kelp supplements or high-iodine diets) can also trigger breakouts.
Should I get blood tests before starting vitamins? If budget and healthcare access allow, baseline labs for vitamin D, B12, zinc, and fasting insulin are valuable—especially for chronic or stubborn hormonal acne that hasn’t responded to basic interventions.
Clearing hormonal acne takes patience and a multi-pronged approach. Start where you are, make incremental changes, and don’t hesitate to seek professional help if your acne is severe or leaving scars. With the right combination of nutrients, habits, and treatments, healthier skin is absolutely within reach.
Click the link if you’re looking for acne support vitamins to help with your overall appearance and learn what ClearB5 can do for you.
- Learn more about Adult Acne Treatment without drugs
Medical Disclaimer
This article is for informational purposes only and does not substitute professional medical advice. Always consult a qualified healthcare provider before starting supplements or changing medical treatment. These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.