Ever notice how your skin seems to have its own opinion about what you ate last weekend? That pizza-and-beer-fueled Saturday might show up as a fresh crop of breakouts by Tuesday. This isn’t just coincidence, it’s your gut talking to your face. The gut health and acne connection is a topic of growing scientific interest, and understanding it can be a game-changer for your skin.
This guide is for anyone struggling with persistent acne who wants to understand the science behind the gut-skin connection. Whether you’re a teen, adult, or someone who’s tried every topical treatment without lasting results, this article is designed for you.
Recognizing this connection can help you address acne from the inside out, not just with topical treatments. By understanding how your gut, immune system, hormones, and skin interact, you can make more informed choices for lasting skin clarity.
Quick Summary: What is the Connection Between Gut Health and Acne?
The connection between gut health and acne lies in the gut-skin axis, a two-way communication system between your digestive tract and your skin. When your gut microbiome (the community of microorganisms living in your digestive tract) is out of balance, it can lead to increased inflammation, hormonal changes, and immune system shifts that show up as acne on your skin. Addressing gut health can help reduce breakouts and improve skin clarity.
FAQ:
Q: What is the connection between gut health and acne?
A: The gut health and acne connection is rooted in the gut-skin axis, where imbalances in your gut microbiome can increase inflammation, disrupt hormones, and alter immune responses, all of which can trigger or worsen acne. Supporting gut health may help reduce breakouts and promote clearer skin.
Key Definitions
- Gut-skin axis: The bidirectional communication network between your digestive system and your skin, involving the immune system, hormones, and microbial metabolites.
- Microbiome: The collection of trillions of microorganisms (bacteria, fungi, viruses) living in and on your body, especially in your gut.
- Intestinal permeability: The ability of the gut lining to control what passes from the digestive tract into the bloodstream. Increased permeability (sometimes called "leaky gut") allows larger molecules and toxins to enter the bloodstream, potentially triggering inflammation.
- Dysbiosis: An imbalance in the gut microbiome, where harmful bacteria outnumber beneficial ones.
- Leaky gut: A lay term for increased intestinal permeability, where the gut barrier becomes less effective at keeping out unwanted substances.
What is Acne, Really?
Understanding Acne: The Basics
Acne vulgaris is a chronic inflammatory disease affecting the pilosebaceous unit—the structure containing your hair follicle and oil gland. While most people associate acne with teenagers, it affects roughly 50 million Americans each year, and studies suggest up to 85% of people between ages 12 and 24 experience some form of acne. Adult acne is increasingly common too, particularly in women in their 20s through 40s.
Types of Acne Lesions
- Noninflammatory lesions: Blackheads (open comedones) and whiteheads (closed comedones) form when dead skin cells and sebum block pores without significant inflammation.
- Inflammatory lesions: Papules, pustules, nodules, and cysts develop when bacteria trigger an immune response, causing redness, swelling, and pain.
Main Drivers of Acne
- Genetics: Set the stage for acne susceptibility.
- Hormones: Androgens, insulin, and IGF-1 (insulin-like growth factor 1, a hormone that promotes cell growth and is linked to increased oil production) can increase oil production and skin cell turnover.
- Excess sebum production: Leads to clogged pores.
- Abnormal skin cell turnover: Causes dead skin cells to accumulate.
- C. acnes overgrowth: Cutibacterium acnes is a bacteria that can trigger inflammation in blocked pores.
Adult Female Patterns
Jawline and chin acne that flares before periods often signals hormonal involvement, a pattern that’s become textbook for adult women struggling with persistent breakouts.
Standard Treatments vs. Gut-Focused Strategies
|
Standard Treatments |
Gut-Focused Strategies |
|---|---|
|
Benzoyl peroxide, topical retinoids, oral antibiotics, hormonal therapies, isotretinoin |
Dietary changes, probiotics, stress management, sleep optimization, fiber-rich foods |
Standard treatments target the skin and bacteria directly, but they can also alter the skin microbiota, particularly by affecting the dominance of Cutibacterium acnes. Changes in the skin microbiota may influence biofilm formation and the expression of virulence factors, which play a role in acne pathology. However, these treatments don’t address what might be happening upstream in your gut, which is why some people see their acne return once they stop treatment, or never fully clear despite trying everything.

Now that you understand what acne is, let’s explore how your gut health influences its development.
Gut Health and Acne: The Quick Answer
Since the early 1900s, researchers have observed that people with acne often have more digestive complaints than those with clear skin. Modern science now explains this through the gut-skin axis, a two-way communication network where your gastrointestinal tract directly influences inflammation, hormones, and even the bacteria living on your face.
Here’s what research consistently shows about the gut health and acne connection:
- Lower intestinal microbiota diversity: Acne patients tend to have fewer types of intestinal microbiota (the diverse community of microorganisms in the gut) compared to people with clear skin.
- Depleted beneficial bacteria: Specifically, reduced levels of Lactobacillus, Bifidobacterium, and other probiotic species that keep inflammation in check.
- Altered bacterial ratios: A higher Bacteroidetes-to-Firmicutes ratio, which is characteristic of Western diet patterns.
- Increased intestinal permeability: More “leaky gut” markers that allow inflammatory compounds to enter the bloodstream.
- Higher systemic inflammation: Elevated inflammatory markers that can amplify skin reactions to Cutibacterium acnes.
In plain language: When your gut is out of balance (dysbiosis, or an unhealthy shift in gut bacteria), inflammatory signals escape into your bloodstream. These signals can ramp up oil production in your sebaceous glands, alter how skin cells behave, and make your immune system overreact to normal skin bacteria, all of which contribute to acne development.
The gut microbiome influences the immune system, which in turn affects skin inflammation and acne development. Hormones and metabolic signals are also affected by gut health, creating a complex web of interactions.
What you can do right now: Focus on fiber-rich foods from diverse plant sources, choose low-glycemic carbohydrates, consider targeted probiotics, and don’t underestimate the power of stress management and quality sleep.
Next, let’s dive deeper into how your gut and skin communicate through the gut-skin axis.
The Gut–Skin Axis: How Your Digestion Talks to Your Face
What is the Gut–Skin Axis?
The gut-skin axis describes a bidirectional communication network where your digestive system and skin constantly exchange signals through your immune system, hormones, nervous system, and microbial metabolites. Think of it as an ongoing conversation—when your gut is happy and balanced, it sends calming messages. When it’s inflamed or disrupted, those alarm signals reach your skin.
- Bidirectional: Signals go both ways, from gut to skin and skin to gut.
- Immune system: Gut bacteria train your immune system; dysbiosis (an imbalance in gut bacteria) can shift you toward a pro-inflammatory state that amplifies acne lesions.
- Hormonal signaling: Your gut microbiota influences insulin sensitivity, androgen metabolism, and estrogen clearance—all relevant to sebum production and skin inflammation.
- Nervous system: The enteric nervous system in your gut communicates with your brain and affects stress responses that impact skin.
- Microbial metabolites: SCFAs (short-chain fatty acids like butyrate, acetate, propionate, which are produced by gut bacteria fermenting fiber), bile acids, and other bacterial products enter circulation and influence distant organs, including your skin microbiome.
A healthy gut microbiome and intact intestinal barrier help regulate the inflammation, oxidative stress, and nutrient absorption that all influence skin conditions. Your gut bacteria produce compounds like short-chain fatty acids (SCFAs), which strengthen your intestinal lining, calm immune reactions, and reduce the low-grade inflammation that can aggravate acne.
What Happens When Things Go Wrong?
When the tight junctions between intestinal cells loosen, a condition often called leaky gut or increased intestinal permeability, bacterial fragments like lipopolysaccharide (LPS, a component of bacterial cell walls that can trigger immune responses) can slip into your bloodstream. This triggers your immune system and creates systemic inflammation that shows up everywhere, including your face. Gut dysbiosis (an imbalance in gut bacteria) and systemic inflammation have been linked to a range of skin diseases, including acne and dermatitis.
Research dating back to 1916 has noted that people with acne report more intestinal issues. Modern studies confirm that markers of intestinal permeability are often elevated in moderate-to-severe inflammatory acne.
Understanding the gut-skin axis helps you see why gut health is so important for clear skin. Next, let’s look at what research says about gut microbes and acne.
What Research Shows About Gut Microbes and Acne
Key Findings
The science connecting gut bacteria to acne has moved beyond speculation into solid territory, though we’re still learning the details.
- Reduced diversity is consistent: Multiple studies show that patients with acne vulgaris have significantly lower gut microbial diversity compared to controls, a pattern seen in other inflammatory and metabolic conditions.
- Specific taxa are depleted: Beneficial gut bacteria like Lactobacillus, Bifidobacterium, Faecalibacterium, and members of the Lachnospiraceae and Ruminococcaceae families are often reduced in patients with acne vulgaris.
- The Firmicutes-Bacteroidetes shift: Patients with acne vulgaris tend to show a higher Bacteroidetes-to-Firmicutes ratio, which is associated with Western dietary patterns and metabolic dysfunction.
- SCFA production matters: Bacteria that ferment fiber into short-chain fatty acids (SCFAs) support gut barrier integrity and anti-inflammatory immune tone. Fewer of these bacteria may mean more leaky gut and more inflammation reaching your skin.
- Emerging causal evidence: A 2024 Mendelian randomization study (a type of genetic analysis that uses genetic variants to determine if an observed association is likely to be causal rather than just correlation) identified 8 gut bacterial taxa, 6 microbial metabolic pathways, and 8 blood metabolites causally associated with acne risk.
One striking finding: elevated blood acetone levels showed an odds ratio of approximately 5.3 for acne development, linking altered ketone metabolism to breakouts. The study also identified mediating pathways where Bifidobacterium influences DHA (an omega-3 fatty acid) levels, which then affect acne risk.
What does this mean for you? Supporting your gut microbes through diet and lifestyle isn’t just wellness fluff, there’s mechanistic evidence that these changes influence the metabolic and inflammatory pathways driving your breakouts.
Next, let’s see how hormones and the gut interact to influence “hormonal” acne.
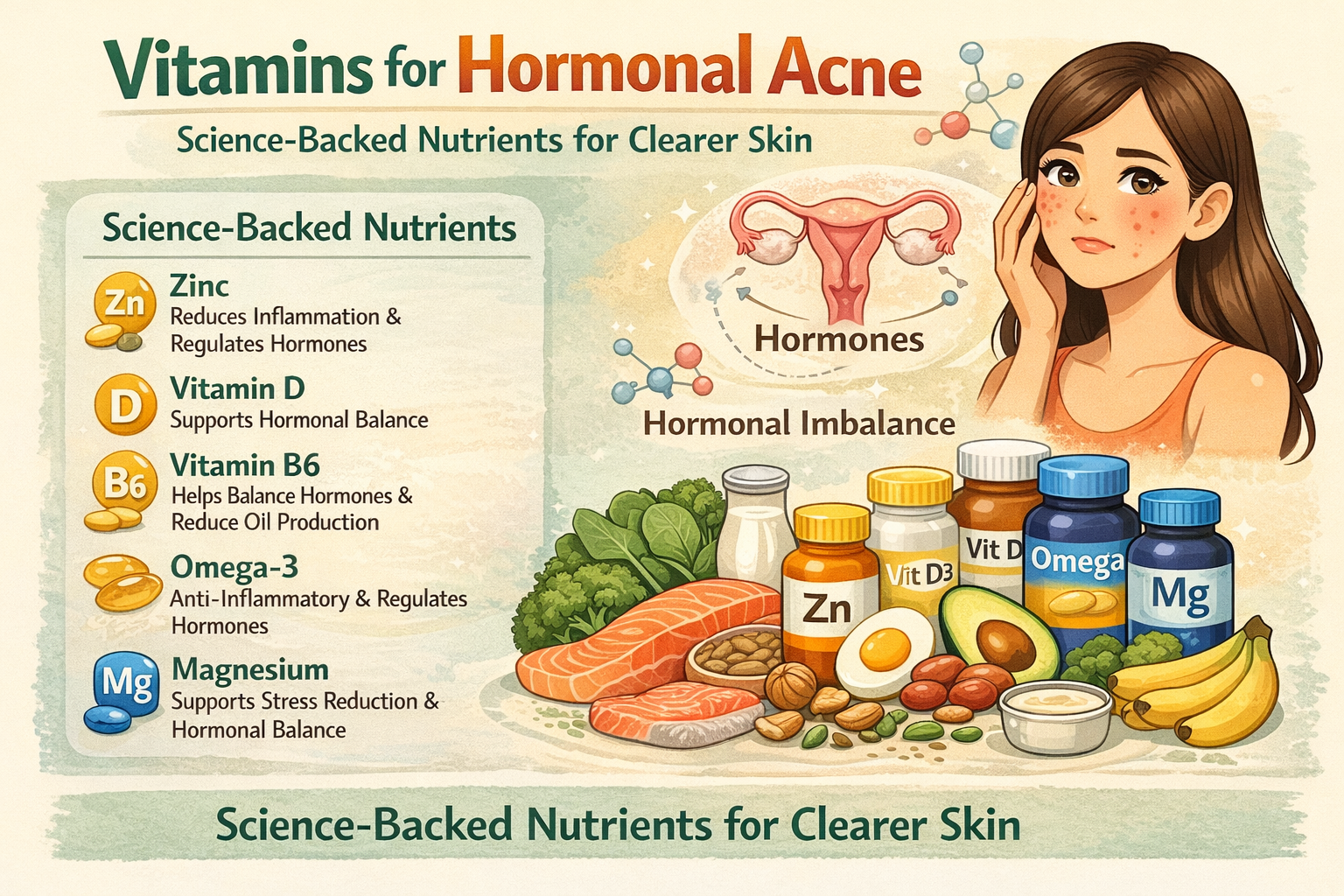
Hormones, Gut Health, and “Hormonal” Acne
How Hormones and Gut Health Interact
If your acne clusters around your jawline and chin, flares predictably before your period, or appeared (or worsened) in your 20s and 30s, you’re likely dealing with what’s commonly called hormonal acne. But here’s the connection most people miss: your gut microbiome plays a significant role in how your body processes hormones.
- The estrobolome: This subset of gut bacteria produces enzymes that metabolize estrogen. When the estrobolome is disrupted, estrogen that your liver tried to clear can get reactivated and recirculated, potentially contributing to hormonal imbalances.
- Beta-glucuronidase activity: Certain gut microbes produce this enzyme, which can “unpackage” estrogen bound for excretion and send it back into circulation—altering your estrogen-to-progesterone ratio.
- Androgen metabolism: Gut dysbiosis and leaky gut are associated with insulin resistance, which increases free androgens (the hormones that drive sebum production and clogged pores).
- Blood sugar and IGF-1: When you eat refined carbohydrates and your blood sugar spikes, insulin and IGF-1 (insulin-like growth factor 1) surge. These activate the mTOR pathway (a cellular signaling pathway that regulates growth and metabolism) in your sebaceous glands and keratinocytes, ramping up oil production and abnormal skin cell turnover.
Summary: The gut microbiome influences hormone metabolism, which in turn affects skin inflammation and acne development.
Transition: Now, let’s see how stress and the gut-brain-skin axis can also impact your breakouts.
Stress, the Gut–Brain–Skin Axis, and Breakouts
How Stress Impacts Your Gut and Skin
Ever noticed your skin freaks out during finals week, before a big presentation, or when you’re running on too little sleep for too long? That’s the gut-brain-skin axis in action, a feedback loop where psychological stress reshapes your gut microbiota composition, increases intestinal permeability, and fuels skin inflammation.
- Stress hormones change your gut: Cortisol and adrenaline alter gut motility, mucus production, and the microbial environment. Beneficial bacteria like Lactobacillus tend to decline under chronic stress.
- Dysbiosis feeds back to inflammation: Stress-driven gut imbalances can increase harmful bacteria and reduce SCFA production, raising inflammatory cytokines that travel to your skin.
- Permeability increases: Chronic stress loosens tight junctions in the intestinal lining, allowing more LPS (lipopolysaccharide, a bacterial fragment that triggers immune responses) and bacterial fragments into circulation.
- The visible result: More red, painful, inflammatory acne during stressful periods—not just “stress picking” but actual physiological changes driving breakouts.
Summary: Stress affects your gut microbiome, which in turn influences your immune system and skin inflammation.

Transition: Next, let’s look at the role of the immune system in acne and how it connects to gut health.
The Role of the Immune System in Acne
How the Immune System Links Gut and Skin
Your immune system is a key player in the story of acne development. When working optimally, it helps defend your skin against harmful bacteria and keeps inflammation in check, supporting healthy skin. But when the immune system is out of balance—often as a result of poor gut health, it can overreact to normal skin bacteria like Cutibacterium acnes (C. acnes), leading to the redness, swelling, and pain that define acne lesions.
An imbalanced immune response doesn’t just make breakouts more likely; it can also increase acne severity. For example, if your immune system is chronically activated due to gut dysbiosis or increased intestinal permeability, it can send inflammatory signals throughout your body, including your skin. This inflammation can trigger or worsen acne, making it harder to achieve clear skin.
Hormonal changes, stress, and even certain foods can further influence your immune system’s behavior, amplifying the cycle of inflammation and breakouts. That’s why supporting your immune system, by nurturing your gut health, managing stress, and eating a balanced diet, can be a powerful strategy for reducing acne development and promoting healthy skin from the inside out.
Transition: Now, let’s identify signs that your gut might be involved in your acne.
Signs Your Gut Might Be Involved in Your Acne
Not all acne traces back to gut issues, genetics, hormones, and skincare habits matter too. However, certain clusters of symptoms raise suspicion that your digestive system deserves attention alongside your skincare routine.
Digestive Symptoms to Watch For
- Frequent bloating, gas, or abdominal discomfort (at least weekly)
- Constipation, diarrhea, or alternating between the two
- Acid reflux or heartburn
- Feeling worse after eating specific foods
Extra-Intestinal Signs Often Linked to Gut Issues
- Persistent fatigue or brain fog
- Strong sugar or carb cravings
- Mood changes, anxiety, or low mood
- Recurrent headaches
Skin Clues Beyond Acne
- Eczema, rosacea, or psoriasis alongside your breakouts
- Skin that’s easily irritated or reactive to foods and stress
- Other inflammatory skin conditions that flare unpredictably
History Factors That Predispose to Gut Dysbiosis
- Multiple antibiotic courses, especially during childhood or for acne treatment
- Long-term NSAID use (ibuprofen, aspirin)
- A diet heavy in ultra-processed foods and light on plants
- Chronic high stress or poor sleep quality
If several of these apply to you, it’s worth exploring the gut connection more seriously. Addressing gut issues and taking steps to reduce inflammation can help improve both digestive and skin symptoms.
Transition: Next, let’s look at what disrupts gut health and could worsen acne.
What Disrupts Gut Health and Could Worsen Acne?
Acne rarely has a single cause. Typically, gut-related contributors stack with genetic predisposition, hormonal fluctuations, and topical skincare factors. Understanding what damages your gut health helps you identify which patterns might be amplifying your breakouts.
Main Disruptors of Gut Health
- Western diet patterns: High in refined carbohydrates, added sugars, processed meats, and seed oils while low in fiber—this eating style reduces microbial diversity and promotes leaky gut.
- Antibiotic use: Both short courses and long-term oral antibiotic therapy for acne can dramatically reduce beneficial gut bacteria and encourage opportunistic overgrowth. Topical antibiotics are also used in acne treatment to target C. acnes bacteria and reduce inflammation, but they should be combined with agents like benzoyl peroxide or retinoids to prevent antibiotic resistance.
- Chronic stress and poor sleep: These shift your microbiome composition, increase intestinal permeability, and raise inflammatory markers.
- Sedentary lifestyle: Lack of regular movement is associated with lower microbial diversity and worse metabolic health.
- Alcohol overuse, smoking, and environmental toxins: All place additional stress on the gut barrier and microbial ecosystem.
None of this is about blame, it’s about recognizing modifiable patterns. Most of us grew up eating processed foods and have taken antibiotics when needed. The point is understanding how these factors accumulate and what you can do now.
Transition: Let’s break down how specific diet patterns can inflame both your gut and your skin.
Diet Patterns That Inflame Both Gut and Skin
Your food choices simultaneously feed your gut bacteria and influence the hormonal and inflammatory pathways driving acne. Some patterns are particularly problematic:
- High-glycemic foods: Soft drinks, candy, white bread, pastries, and sugary cereals spike blood sugar and insulin. Elevated insulin increases IGF-1 and androgen activity, which directly stimulate your sebaceous glands and can trigger acne.
- Ultra-processed foods: Fast food, packaged snacks, instant noodles, and frozen convenience meals often lack the fiber and polyphenols that feed beneficial bacteria. Your gut pathogens may thrive instead.
- Dairy controversies: Some epidemiological studies link skim milk (more than whole milk or fermented dairy) with higher acne risk, possibly due to hormones and whey proteins. But this isn’t universal, some people tolerate dairy fine while others see clear improvement off it.
- Gluten sensitivity: For a subset of people, gluten may contribute to intestinal inflammation and leaky gut, though this isn’t true for everyone.
Practical tip: Rather than following restrictive elimination diets blindly, try keeping a simple food-skin diary for 4-6 weeks. Note what you eat and track your breakouts. Patterns will emerge that are specific to your body.
Choosing fiber-rich, whole foods and minimizing processed foods can support gut health and improve skin outcomes.
Transition: Next, let’s discuss the impact of food sensitivities on acne.
The Impact of Food Sensitivities on Acne
Food sensitivities are often an overlooked factor in acne development and skin health. When your body reacts negatively to certain foods, like dairy, gluten, or processed foods, it can trigger an immune response that leads to inflammation, both in your gut and on your skin. This inflammation can set the stage for breakouts, especially if you’re already prone to acne.
Beyond immediate reactions, food sensitivities can disrupt your gut microbiome, leading to gut dysbiosis. This imbalance in gut bacteria can increase intestinal permeability (sometimes called “leaky gut”), allowing toxins and undigested food particles to slip into your bloodstream. The result? Your immune system ramps up its defenses, which can further increase inflammation and contribute to acne development.
If you suspect food sensitivities are affecting your skin, try keeping a food and symptom diary to identify potential triggers. Eliminating or reducing processed foods and common culprits, then reintroducing them one at a time, can help you pinpoint which foods may be aggravating your acne. By reducing inflammation and supporting a healthy gut microbiome, you can help your skin heal from within.
Transition: Now, let’s look at how managing blood sugar can help keep your skin clear.
Managing Blood Sugar for Clear Skin
Stable blood sugar isn’t just important for your energy and mood—it’s also crucial for clear skin. When blood sugar spikes (often after eating sugary or refined foods), it can trigger a cascade of inflammation and hormonal changes that increase the risk of acne development. High blood sugar can lead to insulin resistance, which in turn raises levels of androgens like testosterone, hormones that stimulate oil production and can clog pores.
A healthy gut microbiome plays a vital role in regulating blood sugar. Eating a healthy diet rich in fiber—think whole grains, fruits, vegetables, legumes, nuts, and seeds—slows the absorption of sugar into your bloodstream, helping to prevent those spikes and crashes that can aggravate acne. Fiber-rich foods also feed beneficial gut bacteria, supporting a healthy gut and reducing inflammation.
To keep your skin clear, focus on balanced meals that combine protein, healthy fats, and plenty of fiber. Limit sugary snacks and processed foods, and aim for steady, consistent eating patterns. By supporting your healthy gut microbiome and managing blood sugar, you’ll be giving your skin the best chance to stay calm, clear, and resilient.
Transition: Next, let’s review how medications, infections, and other factors can disrupt your gut.
Medications, Infections, and Other Gut Disruptors
Beyond diet and lifestyle, certain medical factors can significantly impact your gut microbiota composition:
- Broad-spectrum oral antibiotics: Whether prescribed for acne, sinus infections, or UTIs, these medications don’t discriminate—they reduce beneficial species along with harmful bacteria. Long-term use for acne can foster resistance and persistent dysbiosis.
- Isotretinoin and gut health: Available animal and limited human data don’t show dramatic, consistent gut microbiome damage from isotretinoin, unlike antibiotics. However, some individuals report digestive changes, so monitoring makes sense.
- Common medications: NSAIDs, proton pump inhibitors (PPIs), and some oral contraceptives may influence intestinal permeability or microbial balance in susceptible people.
- Past GI infections: Food poisoning, traveler’s diarrhea, or small intestinal bacterial overgrowth (SIBO) can leave behind long-term imbalances if not fully resolved.
- Antibiotic treatment history: Multiple courses, especially during formative years, may have lasting effects on microbial diversity.
If you have persistent gut symptoms alongside stubborn acne, discuss your medication history with a healthcare professional. Don’t stop prescriptions abruptly, work with your provider to find solutions.
Transition: Now, let’s move on to practical steps for supporting your gut for clearer skin.
How to Support Your Gut for Clearer Skin
Supporting gut health isn’t an overnight cure, but 8-12 weeks of consistent changes often reveal noticeable differences in both digestion and skin. Think of this as a practical roadmap that complements, not replaces, evidence-based dermatology care. The following strategies are designed to improve gut health, which can have a positive impact on skin clarity.
Track Your Progress
- Take weekly skin photos.
- Note digestive symptoms.
- (For women) Track your menstrual cycle.
- This data helps you identify what’s working.
Be Patient
- Microbial shifts take time.
- Don’t expect miracles in week one.
Work with Professionals
- Severe or scarring acne needs dermatological care.
- Gut support is an adjunct, not a replacement.
The Main Pillars We’ll Cover
- Building a microbiome-friendly plate
- Using probiotics and fermented foods wisely
- Reducing leaky gut triggers
- Managing stress, sleep, and lifestyle

Build a Microbiome-Friendly Plate
What you eat directly shapes your gut microbiome within days. Here’s how to build a plate that supports both your digestion and your healthy skin:
- Aim for 25-30+ grams of fiber daily: Get this from diverse sources—vegetables, fruits, legumes, whole grains, nuts, and seeds. Fiber feeds the bacteria that produce anti-inflammatory SCFAs.
- Chase plant diversity: Try to eat 30 different plant foods per week. Different colors and plant types feed different microbial species. This doesn’t have to be complicated—herbs, spices, and seeds all count.
- Choose low-glycemic carbs: Swap white bread and sugary cereals for oats, quinoa, lentils, beans, sweet potatoes, and whole intact grains. These stabilize blood sugar and support insulin sensitivity.
- Include healthy fats: Extra virgin olive oil, avocados, nuts, seeds, and omega-3-rich fish (salmon, sardines, mackerel) provide anti-inflammatory support.
- Limit but don’t obsess: Reduce ultra-processed foods, sugary drinks, and excessive refined vegetable oils, but don’t develop an overly restrictive mindset that adds stress.
Sample Meal Ideas
- Breakfast: Oats with berries, chia seeds, and walnuts
- Lunch: Lentil salad with mixed vegetables and olive oil dressing
- Dinner: Salmon with roasted vegetables and quinoa
- Snacks: Hummus with vegetable sticks, handful of almonds
Use Probiotics and Fermented Foods Wisely
Fermented foods provide live microbes that can help restore balance and support immune function. They’re a food-first approach to improving your gut microbiome:
- Good options: Yogurt with live active cultures, kefir, kimchi, sauerkraut (refrigerated, not shelf-stable), miso, tempeh, and kombucha.
- Strains with some acne data: Lacticaseibacillus rhamnosus, Lactiplantibacillus plantarum, and certain Bifidobacterium species have shown modest benefits in small studies—but results aren’t guaranteed.
- Timing matters: Probiotic supplements may be especially useful during or after antibiotic treatment to support gut resilience.
- Start slowly: Begin with small daily servings to avoid bloating. Monitor your skin response over 6-8 weeks before judging effectiveness.
- Quality counts: If using probiotic supplements, choose products with strain identification, adequate CFU counts, and third-party testing. Work with a health professional for guidance.
Manage Stress, Sleep, and Lifestyle for Your Microbiome
Your daily habits influence your gut microbiome as much as your diet:
- Prioritize sleep: Aim for 7-9 hours consistently. Your gut microbiome follows circadian rhythms, and sleep deprivation disrupts both microbial balance and skin repair processes.
- Build a stress management toolkit: Daily walking, yoga, breathwork, meditation apps, or therapy. Find what works and make it non-negotiable.
- Move regularly: Moderate exercise improves microbial diversity and insulin sensitivity. You don’t need intense workouts, consistent movement matters more.
- Small daily habits: 10-15 minutes of morning sunlight, a wind-down routine before bed, limiting late-night screen exposure.
These aren’t wellness buzzwords, they’re evidence-based interventions that influence the same pathways driving your breakouts.
Transition: Now, let’s answer some of the most common questions about the gut health and acne connection.
Acne, Gut Health, and Specific Questions People Ask
Let’s address some common practical questions about the link between gut health and acne. These answers are educational and don’t replace individualized medical care, especially for severe acne or chronic digestive illness. Emerging therapies that target the gut and skin microbiome are also being explored to treat acne, offering new possibilities for managing this condition.
Should You Cut Out Dairy for Acne?
Dairy is one of the most debated dietary factors in acne. Here’s what the evidence actually shows:
- Skim milk has the strongest association: Several studies link skim milk with higher acne risk, possibly due to hormones and whey proteins. Whole milk, yogurt, and cheese show weaker or no associations.
- Individual variation is huge: Some people notice dramatic improvement off dairy; others see no difference at all. Hard cheeses and fermented dairy (yogurt, kefir) may be better tolerated.
- How to test it: Try a structured 4-6 week reduction, eliminating skim milk, whey protein powders, and ice cream while tracking your skin.
- Replace wisely: Use calcium and vitamin D-fortified plant milks, eat leafy greens, and include canned fish with bones to maintain nutrient intake.
- Reintroduce systematically: Add dairy back gradually and observe whether breakouts return. This gives you personalized data.
Don’t assume dairy is your problem, test it methodically.
Does Accutane (Isotretinoin) Destroy Your Gut?
This question comes up frequently, so let’s look at what we actually know:
- Current evidence is reassuring: Animal research and limited human studies don’t show dramatic, consistent gut microbiome damage from isotretinoin, unlike broad-spectrum antibiotics.
- Individual responses vary: Some people report digestive changes on isotretinoin; others notice nothing different. Monitoring your digestion during treatment is reasonable.
- Isotretinoin is often life-changing: For severe, scarring, or treatment-resistant acne, isotretinoin remains one of the most effective options. Decisions should weigh benefits and risks with your dermatologist.
- Support your gut during treatment: Eat a balanced healthy diet, minimize alcohol (which is already contraindicated with isotretinoin), and consider gentle fermented foods unless they cause issues.
The bottom line: don’t let gut health fears prevent you from considering isotretinoin if you have severe acne. Just support your system during treatment.
Is “Hormonal” Acne Always a Gut Problem?
Not necessarily. Here’s a balanced perspective:
- Hormones are the primary driver: Hormonal acne is driven by androgen activity, insulin signaling, PCOS, menstrual cycles, and sometimes medications—factors that may have nothing to do with your gut.
- But the gut amplifies signals: Gut dysbiosis can worsen insulin resistance, impair estrogen clearance, and raise inflammation—all of which intensify hormonal breakouts.
- Get proper evaluation: Signs of hormonal disorders (irregular periods, excess hair growth, sudden severe acne, unexplained weight changes) warrant medical evaluation. Blood work and possibly imaging may be needed.
- A multi-pronged approach works best: Many people benefit from addressing hormones, gut health, and topical skincare together rather than searching for a single “root cause.”
Hormonal acne rarely has one solution. Tackle it from multiple angles.
When Does It Make Sense to Test Your Gut?
Testing isn’t always necessary, but certain situations make it worthwhile:
Consider testing if you have:
- Chronic digestive symptoms plus stubborn acne that hasn’t responded to conventional treatment
- History of significant gut infections, food poisoning, or traveler’s diarrhea with ongoing symptoms
- Suspected or diagnosed IBD, celiac disease, or autoimmune conditions
- Persistent symptoms despite making dietary and lifestyle changes
What comprehensive stool testing can reveal:
- Microbial diversity scores
- Presence of pathogens or opportunistic organisms
- Inflammatory markers
- SCFA production levels
- Digestive enzyme function
Important caveats:
- Tests like zonulin (a protein that regulates intestinal permeability) and LPS antibodies (which indicate immune response to bacterial fragments) are still evolving and should be interpreted by experienced practitioners.
- Be wary of expensive direct-to-consumer tests promising personalized acne fixes—many lack validation.
- For most people, starting with basic lifestyle changes before testing makes more sense.
If digestive symptoms are minimal and acne is your main concern, invest in dietary changes first. Test if you plateau or have complex symptoms.
Transition: Let’s put all this information together into a clear action plan.
Putting It All Together: Your Gut-Centered Acne Action Plan
Acne reflects a complex interplay of genetics, hormones, the skin microbiome, and gut health through the gut-skin axis and gut-brain-skin axis. Research consistently shows that acne sufferers often have distinct gut microbiota patterns, lower diversity, fewer beneficial bacteria, and more intestinal permeability. Supporting gut balance can reduce systemic inflammation and, for many people, improve skin.
Phased Approach
Weeks 1-4: Foundation
- Focus on low-glycemic, fiber-rich foods and minimize processed foods.
- Drink adequate water.
- Ensure 7-9 hours of sleep nightly.
- Begin a simple food-skin diary.
Weeks 4-8: Layer in Support
- Add fermented foods or targeted probiotic supplements.
- Establish a consistent stress management practice.
- Increase plant diversity toward 30 plants per week.
- Continue tracking skin changes.
Beyond 12 Weeks: Refine and Personalize
- If acne or gut symptoms persist, consider comprehensive testing.
- Work with a dietitian or functional medicine clinician for tailored interventions.
- Reassess your topical skincare and dermatological treatments.
For persistent, scarring, or distressing acne, collaborate with dermatologists, registered dietitians, and integrative medicine practitioners. This isn’t an either/or situation—the best results come from combining evidence-based topical and systemic treatments with gut-focused strategies.
Clear skin often starts in the gut, but sustainable results come from consistent, balanced habits, not quick fixes or extreme elimination diets. Start with one change this week. Add another next week. Give your gut microbiome time to shift, and your skin will likely follow.
Your digestive system and your face are in constant conversation. It’s time to improve what they’re saying to each other.
Click the link if you’re looking for acne support vitamins to help with your overall appearance and learn what ClearB5 can do for you.
- Learn more about Foods that cause acne
Medical Disclaimer
This article is for informational purposes only and does not substitute professional medical advice. Always consult a qualified healthcare provider before starting supplements or changing medical treatment. These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.